The “Unclogging” of Healthcare Delivery
January 2019
HealthCoach- Corporate Wellness
A well-crafted Corporate Wellness Program adapts easily to the digital world of smartphone messaging, wearable biometric data, content delivery and modern wellness strategies.
As we move deeper into the 21st century of healthcare delivery, it has become readily apparent that the epidemic of chronic disease will remain the primary focus of most reform measures by necessity. The United States currently spends 18% of its GDP on healthcare (4,13) and at least 70% of these costs are related to the management of preventable chronic health conditions (6). These costs are projected to double every 25 years, reaching 34% by 2040, and are largely felt to be unsustainable. To respond to this crisis, the United States enacted the Affordable Care Act which seeks to incentivize improved health at a reduced cost through the use of “Big Data” to identify modifiable risk factors in a given population. The “Big Data” approach to achieving cost-effective outcomes is being used in most other industries and healthcare has finally caught on to its potential value.
According to the World Health Organization, 80% of heart disease, stroke, and type 2 diabetes could be prevented and 40% of cancer could be prevented (1). These are the major conditions that are driving increased healthcare costs within the United States. In order to harness the tremendous opportunity to save money by preventing these conditions even before symptoms have appeared, providers will need to shift resources away from costly and risky medical services to less costly and safer preventive services. The United States currently spends 96% on medical services and only 4% on prevention (6).
The United States currently spends 96% on medical services and only 4% on prevention
The Centers for Disease Control reports that the leading drivers of death and disability mostly related to these chronic conditions are poor diet, reduced physical activity, and cigarette smoking. Even though this information has been widely disseminated, less than 3% of the public is following all of the CDC’s recommendations for living a healthy lifestyle (25) and less then 50% are adhering to their medication prescriptions written mostly to stabilize the effects of these lifestyle “risk factors” (37).
This lack of adherence to lifestyle recommendations and to medication prescriptions has resulted in poor control of disease precursors like blood lipids, blood pressure, and blood sugar (targets are being met <50% of the time, 36).
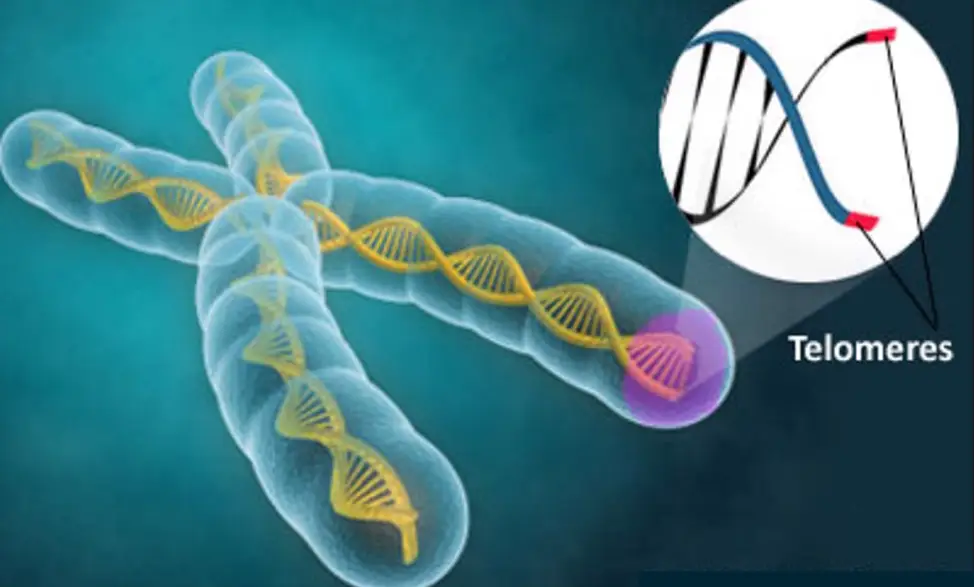
To better understand why lifestyle factors are so important for health, research anthropologists report (21, 20) that the human genetic make-up has changed little in the past 40,000 years and that modern humans are genetically best adapted to:
- Eat natural foods from the earth
- Live outdoors with moderate exposure to the sun
- Live among others in supportive groups
- Sleep when the sun goes down and awaken as the sun comes up
- Walk 5-10 miles each day
- Exhibit a stress response to short-lived stressors and then return to relaxation
They point out that there is a mismatch between how our ancestors lived for 2.5 million years and how we began living only 10,000 years ago after the agricultural revolution (farming, domesticated animals, grains, dairy) and 200 years ago after the industrial revolution (cities, indoor living, decreased family support, decreased physical activity). These mismatches have increased dramatically in the past 30 years:
- Sugar consumption has increased from about 2 pounds per person per year at the beginning of the 20th century to about 150 pounds today (7)
- Processed foods made from refined sugars, cereals, refined vegetable oil, alcohol and dairy products has reached 72% of adult calorie intake (2)
- 79.4% of Americans are physically inactive (3)
- Vitamin D deficiency predominantly from lack of sunlight exposure has reached 82% in some populations (23)
- 18.2 % of the population continues to smoke (6, 3)
- 17.4% of youths age 12-17 use either alcohol or drugs (6, 3)
The best evidence tells us that these mismatches are major contributors to the onset of type 2 diabetes, heart disease, stroke, cancer, Alzheimer’s disease, liver and kidney disease, depression, falls, disability and death (6,1,3,8,9,14,22). These conditions account for most of the chronic disease burden seen around the world and data from the CDC reveals that genetic make-up contributes only 15-18% to the causes of these conditions. The other 80-85% consists of health behaviors, psychosocial factors, and environmental exposures (6, 1).
Our current healthcare system has focused resources mostly on providing care after symptoms, disease, and disability have appeared, instead of focusing on prevention (1,6,19,20,1,11). Healthcare payments tied to fee for service have incentivized care delivery to provide services after blood vessels have become “clogged” (diabetes, coronary heart disease), joints have become arthritic (osteoarthritis, rheumatoid arthritis, lower back pain), and organs have become impaired (cirrhosis, Alzheimer’s disease, kidney failure). Each year in the United States, 2.4 million angiograms, 1 million knee and hip replacements, and 51.4 million medical procedures are carried out (6).
To further frame the problem in the United States:
- We spend 2 ½ times more then the average of our peer nations on healthcare per capita per year (25)
- We rank 37th in overall population health compared to our peer nations (8)
- 77% of those over age 65 have either pre-diabetes or diabetes (9)
- Diabetes accounts for >20% of healthcare costs (9)
- Diabetic patients cost 2.3 times more then non-diabetics each year on average for healthcare (9)
- We rank #1 in the world in prescription drug use (5)
- 76% of every clinical encounter in the U.S. involves a medication (28)
- 80% of the worlds opiate pain pills are prescribed in the United States (27)
- 70% of Americans take one medication, 50% take two, and 20% take five. (26)
- 1/3 of older adults over age 65 fall each year and that increases to 50% for those over age 80 (6)
Now more then ever, we can’t afford to wait for symptoms, disease, or disability to occur before we actively and continuously engage patients in the work of self-care. We need to implement a prevention and wellness delivery system that supports patients in the work of building resiliency by self-managing conditions and lifestyle particularly in between acute episodes of care.
We can’t afford to wait for symptoms, disease, or disability to occur
Our emphasis on pharmaceutical and medical service prescription for chronic disease is unsustainable and has to change if we are to have the necessary resources to maintain our quality of life and our position in the world as a major power. We must now shift to a lower cost prevention and wellness model of care for chronic illnesses and this is exactly what leaders in healthcare innovation are pursuing. By improving health outcomes through this lower cost approach, we could allocate some of these saved resources to other societal problems such as crime, education, poverty and job creation (4).
Our emphasis on pharmaceutical and medical service prescription is unsustainable.
Lessons learned from Medicare’s pioneer ACO pilot programs tell us that we must reduce medical services by preventing “rising risk” patients from becoming “high risk” patients in order for healthcare to become financially viable in the long term (19). This is why the Institute of Medicine, the CDC (6), the Institute for Healthcare Improvement (33), the American Academy of family Physicians (34), and the Centers for Medicare and Medicaid (30) are calling for a shift in care away from reactive disease management to proactive disease prevention.
These organizations are calling for a reorganization of primary care into highly functioning physician-led prevention teams like the patient-centered medical home where each member of the team takes on different responsibilities and works at the top of their license. The team focuses on prevention and wellness of their assigned population and engages patients in the work of self-management.
Self-management support is a KEY intervention for preventing chronic illness (35) but physicians have received little training in team-based care and in condition or lifestyle self-management prescription (38). In addition, both providers and patients have become accustomed to the medication or procedure-based encounter pointing to the additional challenge of creating a “culture” of prevention and wellness (24, 28).
Self-management support is a KEY intervention for preventing chronic illness
Pre-existing models of successful self-management support programs include cardiac rehabilitation (32% improvement in cardiac mortality) (17), pulmonary rehabilitation (37% reduction in acute hospitalizations for COPD) (16), and the diabetes prevention program (70% reduction in onset of diabetes for older pre-diabetic patients) (14).
The Institute of Medicine has recently called for medical education reform to meet the new demand for prevention and wellness delivery within primary care (10) but this could take many years to implement once medical schools finally embrace these recommendations.
To further elucidate the healthcare “cultural” problem, patients report that they would rather take medications or undergo surgery then make changes in their health behaviors to reduce chronic disease risk factors (24). In order to change this paradigm, the American Hospital Association has called for the enactment of a “culture of wellness” throughout our systems of care (29).
They recognize that the cultural disconnect between the OLD way of reactive care delivery and the NEW way of preventive care delivery. Changing culture takes time and this will be a significant challenge for 21st century healthcare. The providers who succeed in making this cultural shift sooner then later will be the winners within the NEW value-based payment system that is emerging (19).
Patients report that they would rather take medications or undergo surgery then make changes in their health behavior
Leaders from the Robert Wood Johnson Foundation (11), from Kaiser-Permanente (31), from Cleveland Clinic (32) and many other integrated care systems (18) are working to prevent disease at every level within the chronic disease lifecycle. They are calling for prevention and wellness integration as a primary focus for better outcomes delivery at a reduced cost. This is consistent with Medicare’s triple aim vision for the future of healthcare (18).
With the shift to electronic medical records and the push to get patients “into the system”, more providers will be able to use BIG DATA to identify the right risks for prevention so that limited resources can be targeted in the right way. This is what the Robert Wood Johnson foundation calls “A Prescription for Health” (12) and this is what will sustain healthcare delivery in the long term.
HealthCoach – tracks biomarker information like steps per day, weight (loss or gain), BMI, continuous blood sugar, sleep, hydration and food choices – as well as a host of other cohorts through fitness tracking technology.
HealthCoach – allows doctors, participants and health coaches to use secure HIPAA messaging or video conferencing to help with better food choices, to encourage consistent steps per day, to insure safe weight loss and to communicate data back to the doctor for reassessment every 90 days.
References:
- Preventing chronic diseases: a vital investment WHO, 2005
- Origins and evolution of the Western diet: Health implications for the 21st century, Loren Cordain, Am J Clin Nutr, February 2005
- Healthypeople.gov
- Congressional Budget Office, 2009
- Extent and causes of international variations in drug usage. A report for the Secretary of State for Health. July, 2010, UK
- The Power of Prevention: The Public health Challenge of the 21st Century, CDC 2009
- USDA.gov
- The State of U.S. Health, 1990-2010, JAMA, July 2013
- Diabetes Fact Sheet, 2011, CDC.gov
- Interview Gail Wilensky, Institute of Medicine Co-chair, Committee on the Governance and Financing of Graduate Medical education, July 2014
- Interview with James Marks, Director of Program Portfolios, RWJF, US 1 Magazine, Princeton, N.J.
- Prescriptionforhealth.org
- Council of Economic Advisors, Whitehouse.gov
- Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin, Diabetes Prevention research Group, NEJM; Vol 346:6, 394-403
- Institute of Medicine. Preventing Medication Errors: Quality Chasm Series, Washington, DC: National Academy Press; 2007.
- Olivia Revitt, Louise Sewell et. al., Short outpatient pulmonary rehabilitation program reduces readmission following a hospitalization for an exacerbation of chronic obstructive pulmonary disease, Respirology, Volume 18, Issue 7, pages 1063–1068, October 2013
- Rod S. Taylor, Allan Brown et al., Exercise-Based Rehabilitation for Patients with Coronary Heart Disease: Systemic Review and Meta-analysis of Randomized Controlled Trials, Am J Med 2004; 116: 682-692
- http://innovation.cms.gov/
- Population Health, Healthcare Informatics Webinar, Advisory Board Research, March 2014
- S. Boyd Eaton, Beverly I. Strassman, Randolph Nesse et al., Evolutionary Health Promotion, Preventive Medicine 34, December 2001, 109-118
- Evolution in Health and Disease (Oxford Biology): January 10, 2008 by Stephen C. Stearns and Jacob C. Koella
- Dale Bredesen, Reversal of cognitive decline: A novel therapeutic program, AGING, September 2014, Vol 6 N 9
- Forrest KY1, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011 Jan;31(1):48-54.
- Allan S. Detsky M.D., PhD, What patients really want from health care? JAMA, December 14, 2011, Vol 306, No. 22
- OECD Health Data, 2012
- May Clinic Proceedings, June 2013
- ABC News, April 20, 2011
- CDC Faststats, 2013
- A Call to Action: Creating a Culture of Health, American Hospital Association, January 2011
- CMS Comprehensive Primary Care Initiative, June 2012 Webinar
- Healthcare Will Note Reform Itself, George Halvorson, CEO Kaiser Permanente, 2009
- The Cleveland Clinic Way: Lessons in Excellence from One of the World’s Leading Health Care Organizations Hardcover – January 7, 2014 by Toby Cosgrove
- Institute for Healthcare Improvement, triple Aim for Populations, http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx
- American Academy of family Physicians, Summary of Recommendations for Clinical Preventive Services, November 2014
- Mary Thoeson Coleman, Karen S. Newton, Supporting Self-management in Patients with Chronic Illness, American Family Physician, 2005 Oct 15; 72 (8): 1503-1510
- Cardio metabolic Health Congress, Statement of Need, http://www.cardiometabolichealth.org/2013/accreditation.asp
- Top 10 Prescription Drugs in the U.S., Institute for Healthcare Informatics, 2010
- Doctors and Patients, Not Talking About Weight, New York Times, March 16, 2010
- Stephen B. Lewis M.D., FABPMR