More than 29 million people in the US have diabetes, a staggering one in four don’t know they suffer from it and K6 children are developing prediabetes at alarming rates.
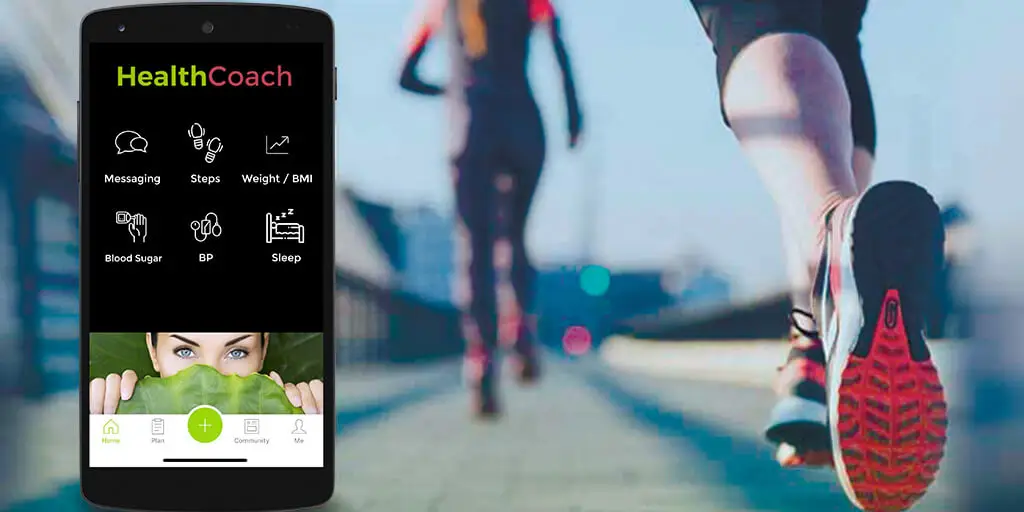
For those who do, how you regularly track glucose data depends on the type of diabetes one has and the treatment required. Monitoring is commonly done by taking a drop of blood with a pinprick, but a lot of people track continuously with wearables that measure blood sugar at intervals and relay that information to a smartphone or other device. (HealthCoach)
The first option is unpleasant and often inconvenient; the second is costly, and still invasive – but there is hope for diabetics to live more comfortable lives in the future with continuous glucose monitoring.
Non-invasive testing, where the skin isn’t penetrated at all, is the key to glucose monitoring.
Dexcom is one of the biggest names in continuous glucose monitoring with devices used by 200,000 people worldwide. Dexcom’s wearable tracker is made of two parts: a disposable needle that goes just under the skin to monitor interstitial fluid; and a patch that sits on top, housing the electronics that measure the sensor and transmit them to a Bluetooth device.
Most continuous trackers on the market read from this interstitial fluid, as blood glucose diffuses very quickly into it, making it highly indicative of exact levels at any given time. The latest Dexcom device, the G6 is slightly different then the G5.
The G5 and G6 is worn on the upper abdomen and Dexcom boasts that it’s the only one on the market that lets people make treatment decisions from the information. Dexcom states that readings from the device can determine if people should eat carbohydrates or take their insulin which is very unique because competitive devices don’t have that same level of performance.
The G5 is primarily used for patients with Type 1 diabetes, or who intensively manage their diabetes with insulin, but that Dexcom G5 and new G6 is also starting to see some usage by Type 2 sufferers and can be used by a HealthCoach – Gerald J. Joseph
- 442 million people worldwide have diabetes
- Sufferers of type 1 diabetes have a lack of insulin production, while in type 2 the body gradually becomes resistant to the insulin it can make
- According to WHO data, diabetes was the sixth leading cause of death globally in 2015,
Overall- the new G6 improves on many fronts over G5, particularly the outstanding new one-button sensor inserter (applicator), strong accuracy without any finger-stick calibrations (maintaining a short two-hour warmup period), an extension to 10-day wear, a slimmer on-body Bluetooth transmitter, and clearance for use with other diabetes devices under an exciting new FDA pathway.
Compared to the G5, which had 7-day sensor wear, the G6 is expected to be more economical due to the longer 10-day wear
HealthCoach will be using the G6 to gather biometric data (blood sugar) in addition (steps, hydration, sleep, BMI, weight) Gerald J. Joseph says – a continuous tracker like the Dexcom G6 will be able to get better analytics to support people to make chronic disease management decisions in real-time – without the inconvenience of daily blood pricks and to communicate with the doctor – nurse – HealthCoach – “data” in a collaborative process in making lifestyle changes.
Dexcom’s G5 and G6 is currently only FDA approved for abdominal use, but soon smart watches may one day perform the same task?
Continuous Glucose Monitors
Like other CGMs – future watches will penetrate the skin to the interstitial space, but with an interchangeable module which will need to be changed once a month, that sits on the back of the watch and pushes the biochemical sensors under the skin. The accuracy rate is at +/- 8%, however it is yet to get the clearance from health regulators to put it in the hands of consumers.
HealthCoach – People with diabetes incur medical costs about 2.3 times higher than those who don’t suffer from the disease.
Non-Invasive Methods – HealthCoach
Sweat contains a small amount of glucose which is derived from blood and interstitial fluid -researchers believe thatsweat glands which are distributed throughout the body could reflect dynamic physiological conditions of body which can help in real time a “HealthCoach” champion lifestyle changes “Gerald J. Joseph” says.
Because the correlation of glucose in sweat is much lower than that in the blood, sensitive sensors must become more accurate to match the accuracy of a direct reading of interstitial fluid or blood.
The correlation between sweat and blood glucose also needs to be studied more thoroughly
As for what the future holds – wearable glucose tracking is coming! For Diabetics, there are other factors to consider than just keeping an eye on their blood.
They are at risk for neuropath – open wounds damaging nerves and more prone to foot injuries that don’t heal easily. Early detection is essential and I foresee in the future socks helping the doctor – healthcoach detect increased blood sugar levels.
Our bodies respond to injury with inflammation, which causes heat; socks in the future will alert the wearer with a notification on their smartphone (HealthCoach) when they detect rising temperature in specific areas of the foot.
For proper diabetic foot care, I recommend wearing fresh cotton white socks and replace socks every month to avoid thinning especially with patients who have lost a toe or have had multiple ulcers – in addition to consuming my HealthCoach diet.
Detecting SUGAR
Detecting a massive intake of sugar levels in real time can help you see what sugary foods do to your body in real time – maybe you’ll be less likely to reach for a soda, or even a donut or cookie and just maybe the next time you may choose a delicious whole fruit snack.
More specifically non-invasive continuous glucose monitoring can essentially track your glucose levels just like wearables track your heart rate now. You’d have a daily, minute-by-minute break down throughout your day and no when you’ve been naughty.
You, your doctor and or your HealthCoach could then better and more instantly tweak your diet. And since diet is half of maintaining a healthy lifestyle, it could completely change people’s lives.
There are different levels of glucose monitoring.
Non-invasive continuous glucose monitoring would more likely impact everybody, largely because you’d get that near-instant feedback loop between what you eat and how your glucose is affected.
The level below that is just non-invasive glucose monitoring – this would allow something like a fitness tracker to track your glucose, but not all the time – perhaps at hourly intervals. It would be nice, but it’s not as game-changing as continuous glucose monitoring.
Let’s also not forget that there are around 100 million Americans living with diabetes. Non-invasive glucose monitoring would be a major quality-of-life upgrade, saving them a prick on the finger.
It’s one thing to be able to do non-invasive continuous glucose monitoring, it’s another thing to be able to do it so well it can help advise on insulin dosage for those with diabetes.
Let’s Look Deeper – The Science
The problem is really about the laws of physics – you simple can not draw that much data from things like interstitial fluid at this time – More on this and how the Gerald J. Joseph – HealthCoach Prevention Program (HCPP) affects blood sugar (HbA1c)- in part II.
It does look like Continuous Non-Invasive Glucose Monitoring seems to actually be working and finally doctors and patients are going see how a can of Coke, grains and or processed foods affects blood sugar.
HEALTHCOACH 2020