Weight Loss Success Linked to Telehealth Coaching, mHealth Devices.
A new study finds that a TeleHealth platform offering one-on-one coaching and an mHealth App connected to wireless devices can lead to “significant” reductions in weight and body mass and an increase in activity for those struggling with obesity.
As reported in the Journal of Telemedicine and Telecare, a 12-week weight loss program that included weekly video visits with a healthcoach and an mHealth App linked to a Bluetooth-enabled wireless scale, blood pressure monitor and accelerometer resulted in clinically significant weight-loss for almost 70 percent of the participants.
By contrast, a control group with access to the same wireless devices but not weekly telehealth coaching sessions saw only 8 percent of participants losing a significant amount of weight, and there was a “significant difference” in both body weight-loss and percent body weigh-loss between the two groups.
https://mhealthintelligence.com/news/weight-loss-success-linked-to-telehealth-coaching-mhealth-devices
Gerald J. Joseph International, LLC
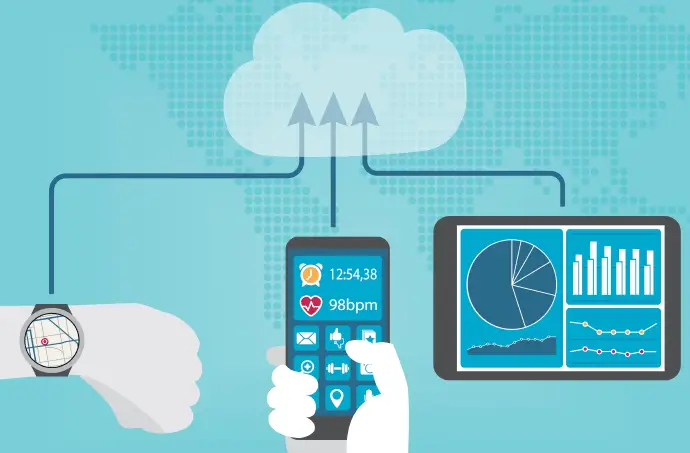
Imagine you could go about your day and all the while a device you wear on your wrist or the phone you are holding, is sending data to your personal HealthCoach to help you make better dietary and physical activity decisions, decisions that can help you to be the best, healthiest version of yourself.
The Gerald J. Joseph HealthCoach Program does exactly that.
The Gerald J. Joseph HealthCoach Program uses an all-in-one HealthCoach App that stores a user’s data, and sends biometric information from a wearable device for real-time assessment and allows a HealthCoach to monitor a client’s progress and give real-time feedback. Using this app, a HealthCoach can improve clients’ health outcomes and reduce healthcare costs for client and provider alike.
HealthCoach App
The App is rich in communications abilities. It allows a client to upload health-related files (HIPPA compliant), and also provides links for educational video content and secure messaging.
The App can be programmed to track basic information like steps per day, weight (loss or gain), blood sugar, sleep, and hydration as well as a host of other cohorts. On the simplest level, tracking only steps and weight, the App can be used by Health Coaches to help clients with weight loss, Type II Diabetes, program compliance, and basic fitness levels.
The App helps individual Health Coaches communicate with their clients, and it is scalable. A single HealthCoach can oversee the progress of 100-150 clients, and we anticipate scaling the program to accommodate any number of clients. The software also allows for a supervisor to monitor the progress of the Health Coaches, and to help guide them to best assist their clients.
TeleHealth
Telehealth is one of the fastest growing segments of the healthcare industry – the American Medical Association reports that 70 percent of all healthcare visits could have been done virtually.
Gerald J. Joseph International, LLC has developed a cloud-based HealthCoach program aimed at reducing employers’ overall medical spending, reducing accidents, improving productivity, and improving return-to-work outcomes by engaging employees with a digital HealthCoach App based wellness program to improve health outcomes.
The Gerald J. Joseph HealthCoach Program shifts the focus onto the success of the employee active participation in improving nutrition, mobility and perception of their improved health.
The Gerald J. Joseph HealthCoach Program uses a validated “Motivational Interviewing” (MI) tool to assess the fidelity of wellness, disease management or care management services for evidence-based health coaching best practices.
HealthCoach
As your “HealthCoach“, I communicate with you via text, email and phone 24/7 to help you achieve the benefits of a well-designed diet and exercise program. I answer questions, I interface with your medical doctor, I provide wellness insights, I empower you, help you evaluate lab results, and help you steer toward the outcome you have stated when you began working with me.
Most of my adult life has been spent in the pursuit of knowledge to help people live better, more fulfilling disease free lives, through proper evidence-based nutrition and exercise.
Gerald J. Joseph, B.S., M.Ed.